ALL ABOUT EBOLA VIRUS
Ebola virus disease
From Wikipedia, the free encyclopedia
"Ebola" redirects here. For other uses, see Ebola (disambiguation).
| Ebola virus disease | |
|---|---|
| Classification and external resources | |
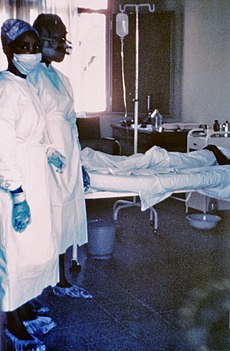
1976 photograph of two nurses standing in front of Mayinga N., a person with Ebola virus disease; she died only a few days later due to severe internal hemorrhaging.
|
|
| ICD-10 | A98.4 |
| ICD-9 | 065.8 |
| DiseasesDB | 18043 |
| MedlinePlus | 001339 |
| eMedicine | med/626 |
| MeSH | D019142 |
The virus may be acquired upon contact with blood or bodily fluids of an infected animal (commonly monkeys or fruit bats).[1] Spread through the air has not been documented in the natural environment.[2] Fruit bats are believed to carry and spread the virus without being affected. Once human infection occurs, the disease may spread between people as well. Male survivors may be able to transmit the disease via semen for nearly two months. In order to make the diagnosis, typically other diseases with similar symptoms such as malaria, cholera and other viral hemorrhagic fevers are first excluded. Blood samples may then be tested for viral antibodies, viral RNA, or the virus itself to confirm the diagnosis.[1]
Prevention includes decreasing the spread of disease from infected monkeys and pigs to humans. This may be done by checking such animals for infection and killing and properly disposing of the bodies if the disease is discovered. Properly cooking meat and wearing protective clothing when handling meat may also be helpful, as are wearing protective clothing and washing hands when around a person with the disease. Samples of bodily fluids and tissues from people with the disease should be handled with special caution.[1]
There is no specific treatment for the disease; efforts to help persons who are infected include giving either oral rehydration therapy (slightly sweet and salty water to drink) or intravenous fluids.[1] The disease has high mortality rate: often killing between 50% and 90% of those infected with the virus.[1][3] EVD was first identified in Sudan and the Democratic Republic of the Congo. The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] From 1976 (when it was first identified) through 2013, fewer than 1,000 people per year have been infected.[1][4] The largest outbreak to date is the ongoing 2014 West Africa Ebola outbreak, which is affecting Guinea, Sierra Leone, Liberia and likely Nigeria.[5][6] As of July 2014 more than 1320 cases have been identified.[5] Efforts are ongoing to develop a vaccine; however, none yet exists.[1]
Signs and symptoms

Symptoms of Ebola.[7]
Bleeding
In the bleeding phase, internal and subcutaneous bleeding may present itself through reddening of the eyes and bloody vomit.[8] Bleeding into the skin may create petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites).All people infected show some symptoms of circulatory system involvement, including impaired blood clotting.[10] Bleeding from puncture sites and mucous membranes (e.g. gastrointestinal tract, nose, vagina and gums) is reported in 40–50% of cases.[11] Types of bleeding known to occur with Ebola virus disease include vomiting blood, coughing it up or blood in the stool. Heavy bleeding is rare and is usually confined to the gastrointestinal tract.[10][12] In general, the development of bleeding symptoms often indicates a worse prognosis and this blood loss can result in death.[13]
Causes
Main article: Ebolavirus
EVD is caused by four of five viruses classified in the genus Ebolavirus, family Filoviridae, order Mononegavirales. These four viruses are Bundibugyo virus (BDBV), Ebola virus (EBOV), Sudan virus (SUDV), Taï Forest virus (TAFV). The fifth virus, Reston virus
(RESTV), is not thought to be disease-causing in humans. During an
outbreak, those at highest risk are health care workers and close
contacts of those with the infection.[14]Transmission
It is not entirely clear how Ebola is spread.[15] EVD is believed to occur after an ebola virus is transmitted to an initial human by contact with an infected animal's body fluids. Human-to-human transmission can occur via direct contact with blood or bodily fluids from an infected person (including embalming of an infected dead person) or by contact with contaminated medical equipment, particularly needles and syringes.[16] Semen is infectious in survivors for up to 50 days. Transmission through oral exposure and through conjunctiva exposure is likely[17] and has been confirmed in non-human primates.[18] The potential for widespread EVD infections is considered low as the disease is only spread by direct contact with the secretions from someone who is showing signs of infection.[16] The quick onset of symptoms makes it easier to identify sick individuals and limits a person's ability to spread the disease by traveling. Because dead bodies are still infectious, some doctors disposed of them in a safe manner, despite local traditional burial rituals.[19]Medical workers who do not wear appropriate protective clothing may also contract the disease.[20] In the past, hospital-acquired transmission has occurred in African hospitals due to the reuse of needles and lack of universal precautions.[21]
Airborne transmission has not been documented during previous EVD outbreaks.[2] They are, however, infectious as breathable 0.8–1.2 micrometre laboratory generated droplets;[22] because of this potential route of infection, these viruses have been classified as Category A biological weapons.[23] Recently the virus has been shown to travel without contact from pigs to non-human primates.[24]
Bats drop partially eaten fruits and pulp, then land mammals such as gorillas and duikers feed on these fallen fruits. This chain of events forms a possible indirect means of transmission from the natural host to animal populations, which has led to research towards viral shedding in the saliva of bats. Fruit production, animal behavior, and other factors vary at different times and places that may trigger outbreaks among animal populations.[25]
Reservoir
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians, and arthropods sampled from outbreak regions, no ebolavirus was detected apart from some genetic traces found in six rodents (Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic.[28][34] Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high lethality from infection in these species makes them unlikely as a natural reservoir.[28]
Transmission between natural reservoir and humans is rare, and outbreaks are usually traceable to a single case where an individual has handled the carcass of gorilla, chimpanzee, or duiker.[35] Fruit bats are also eaten by people in parts of West Africa where they are smoked, grilled or made into a spicy soup.[32][36]
Virology
Main article: Ebola virus
Genome
Like all mononegaviruses, ebolavirions contain linear nonsegmented, single-strand, non-infectious RNA genomes of negative polarity that possesses inverse-complementary 3' and 5' termini, do not possess a 5' cap, are not polyadenylated, and are not covalently linked to a protein.[37] Ebolavirus genomes are approximately 19 kilobase pairs long and contain seven genes in the order 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[38] The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV, and TAFV) differ in sequence and the number and location of gene overlaps.Structure
Like all filoviruses, ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched.[38] In general, ebolavirions are 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974 to 1,086 nm (in contrast to marburgvirions, whose median particle length was measured at 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture.[39]Replication
The ebolavirus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol. The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is, therefore, a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-strand antigenomes that are, in turn, transcribed into negative-strand virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.[40]Pathophysiology
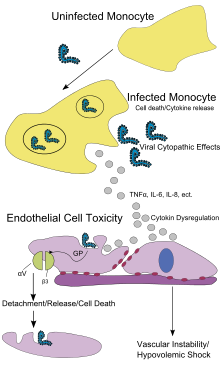
Endothelial cells, mononuclear phagocytes, and hepatocytes are the main targets of infection. After infection, a secreted glycoprotein (sGP) known as the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a trimeric complex, which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a dimeric protein that interferes with the signaling of neutrophils, a type of white blood cell, which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen.[41]The presence of viral particles and cell damage resulting from budding causes the release of cytokines (to be specific, TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.[42]
Diagnosis
The medical history, especially travel and work history along with exposure to wildlife are important to suspect the diagnosis of EVD. The diagnosis is confirmed by isolating the virus, detecting its RNA or proteins, or detecting antibodies against the virus in a person's blood. Isolating the virus by cell culture, detecting the viral RNA by polymerase chain reaction (PCR) and detecting proteins by enzyme-linked immunosorbent assay (ELISA) is effective early and in those who have died from the disease. Detecting antibodies against the virus is effective late in the disease and in those who recover.[43]During an outbreak, virus isolation is often not feasible. The most common diagnostic methods are therefore real time PCR and ELISA detection of proteins, which can be performed in field or mobile hospitals.[44] Filovirions can be seen and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot tell the difference between the various filoviruses despite there being some length differences.[39]
Classification

Phylogenetic tree comparing the Ebolavirus and Marburgvirus. Numbers indicate percent confidence of branches.
Rates of genetic change are 100 times slower than influenza A in humans, but on the same magnitude as those of hepatitis B. Extrapolating backwards using these rates indicates that Ebolavirus and Marburgvirus diverged several thousand years ago.[46] However, paleoviruses (genomic fossils) of filoviruses (Filoviridae) found in mammals indicate that the family itself is at least tens of millions of years old.[47] Fossilized viruses that are closely related to ebolaviruses have been found in the genome of the Chinese hamster.[48]
Differential diagnosis
The symptoms of EVD are similar to those of Marburg virus disease.[49] It can also easily be confused with many other diseases common in Equatorial Africa such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis. Other infectious diseases that should be included in the differential diagnosis include the following: leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, hemorrhagic smallpox, measles, and fulminant viral hepatitis.[citation needed] Non-infectious diseases that can be confused with EVD are acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and even warfarin poisoning.[50][51][52][53]Prevention

A researcher working with the Ebola virus while wearing a BSL-4 positive pressure suit to avoid infection
Behavioral changes
Ebola viruses are contagious, with prevention predominantly involving behavior changes, proper full-body personal protective equipment, and disinfection. Techniques to avoid infection involve not contacting infected blood or secretions, including from those who are dead.[15] This involves suspecting and diagnosing the disease early and using standard precautions for all patients in the healthcare setting.[54] Recommended measures when caring for those who are infected include isolating them, sterilizing equipment, and wearing protective clothing including masks, gloves, gowns and goggles.[15] Hand washing is important but can be difficult in areas where there is not even enough water for drinking.[13]Due to lack of proper equipment and hygienic practices, large-scale epidemics have occured mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Traditional burial rituals, especially those requiring embalming of bodies, should be discouraged or modified.[54] Airline crews who fly to these areas of the world are taught to identify Ebola and isolate anyone who has symptoms.[55]
Quarantine
Quarantine, also known as enforced isolation, is usually effective in decreasing spread.[56][57] Governments often quarantine areas where the disease is occurring or individuals who may be infected.[58] In the United States the law allows quarantine of those infected with Ebola.[59] The lack of roads and transportation may help slow the disease in Africa. During the 2014 outbreak Liberia closed schools.[60]Vaccine
No vaccine is currently available for humans.[1][61][62] The most promising candidates are DNA vaccines[63] or vaccines derived from adenoviruses,[64] vesicular stomatitis Indiana virus (VSIV)[65][66][67] or filovirus-like particles (VLPs)[68] because these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.[69][70][71][72]Vaccines have protected nonhuman primates. Immunization takes six months, which impedes the counter-epidemic use of the vaccines. Searching for a quicker onset of effectiveness, in 2003 a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein was tested on crab-eating macaques. Twenty-eight days later they were challenged with the virus and remained resistant.[64] A vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or the Marburg glycoprotein in 2005 protected nonhuman primates,[73] opening clinical trials in humans.[69] The study by October completed the first human trial, over three months giving three vaccinations safely inducing an immune response. Individuals for a year were followed, and, in 2006, a study testing a faster-acting, single-shot vaccine began; this new study was completed in 2008.[70] Trying the vaccine on a strain of Ebola that more resembles one that infects humans is the next step.[citation needed]
On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak.[74] An experimental vaccine made by researchers at Canada's national laboratory in Winnipeg was used in 2009 to pre-emptively treat a German scientist who might have been infected during a lab accident.[75] However, actual EBOV infection could never be demonstrated without a doubt.[76] Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis.[77][78][clarification needed]
Laboratory
Ebola viruses are World Health Organization Risk Group 4 pathogens, requiring biosafety level 4-equivalent containment. Laboratory researchers must be properly trained in BSL-4 practices and wear proper personal protective equipment.Treatment
No ebolavirus-specific treatment exists.[62] Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control bleeding, maintaining oxygen levels, pain management, and the use of medications to treat bacterial or fungal secondary infections.[79][80][81] Early treatment may increase the chance of survival.[82] A number of experimental treatments are being studied.Prognosis
The disease has a high mortality rate: often between 50 percent and 90 percent.[1][3] If an infected person survives, recovery may be quick and complete. Prolonged cases are often complicated by the occurrence of long-term problems, such as inflammation of the testicles, joint pains, muscle pains, skin peeling, or hair loss. Eye symptoms, such as light sensitivity, excess tearing, iritis, iridocyclitis, choroiditis and blindness have also been described. EBOV and SUDV may be able to persist in the semen of some survivors for up to seven weeks, which could give rise to infections and disease via sexual intercourse.[1]Epidemiology
For more about specific outbreaks and their descriptions, see List of Ebola outbreaks.
The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] From 1976 (when it was first identified) through 2013, fewer than 1,000 people per year have been infected.[1][4] The largest outbreak to date is the ongoing 2014 West Africa Ebola outbreak, which is affecting Guinea, Sierra Leone, and Liberia.[5] As of August 2014 it is also affecting Nigeria.[6] As of the end of July 2014 more than 1320 cases have been identified.[5]2007 to 2011
As of 30 August 2007, 103 people (100 adults and three children) were infected by a suspected hemorrhagic fever outbreak in the village of Kampungu, Democratic Republic of the Congo. The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The World Health Organization sent a team to take blood samples for analysis and confirmed that many of the cases were the result of Ebolavirus.[83][84] The Congo's last major Ebola epidemic killed 245 people in 1995 in Kikwit, about 200 miles (320 km) from the source of the August 2007 outbreak.[85]On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of Ebolavirus, which was tentatively named Bundibugyo.[86] The epidemic came to an official end on 20 February 2008. While it lasted, 149 cases of this new strain were reported, and 37 of those led to deaths.
An International Symposium to explore the environment and filovirus, cell system and filovirus interaction, and filovirus treatment and prevention was held at Centre Culturel Français, Libreville, Gabon, during March 2008.[87] The virus appeared in southern Kasai Occidental on 27 November 2008,[88] and blood and stool samples were sent to laboratories in Gabon and South Africa for identification.
On 25 December 2008, it was reported that the Ebola virus had killed 9 and infected 21 people in the Western Kasai province of the Democratic Republic of Congo.[89] On 29 December, Doctors Without Borders reported 11 deaths in the same area, stating that a further 24 cases were being treated. In January 2009, Angola closed down part of its border with the Democratic Republic of Congo to prevent the spread of the outbreak.[90]
On 12 March 2009, an unidentified 45-year-old scientist from Germany accidentally pricked her finger with a needle used to inject Ebola into lab mice. She was given an experimental vaccine never before used on humans. Since the peak period for an outbreak during the 21-day Ebola incubation period had passed as of 2 April 2009, she had been declared healthy and safe. It remains unclear whether or not she was ever actually infected with the virus.[91]
In May 2011, a 12-year-old girl in Uganda died from Ebola (Sudan subspecies). No further cases were recorded.[92]
2012 outbreaks
In July 2012, the Ugandan Health Ministry confirmed 13 deaths due to an outbreak of the Ebola-Sudan variant[93] in the Kibaale District.[94] On 28 July, it was reported that 14 out of 20 (70% mortality rate) had died in Kibaale.[95] On 30 July, Stephen Byaruhanga, a health official in Kibaale District, said the Ebola outbreak had spread from one remote village to several villages.[96]The World Health Organization's (WHO) global and alert response network reported on 3 August that the suspected case count had risen to 53, including 16 deaths. Of these cases, five were confirmed by UVRI as Ebola cases. There were no confirmed cases outside of Kibaale District except for a patient who was medically evacuated to Kampala District and then died. WHO and CDC support was on the ground in Uganda supporting the government response. There were no confirmed cases outside of Uganda.[97] Included among populations confirmed to be affected were prisoners in Kabbale prison. [98] Dr. Joaquim Saweka, the WHO representative to Uganda, reported that the outbreak was under control and that everyone known to have had contact with a known Ebola patient was in isolation.[99]
On 8 August, the Ugandan Ministry of Health recorded 23 probable and confirmed cases, including 16 deaths. Ten cases were confirmed by the Uganda Virus Research Institute as Ebola. 185 people who came into contact with probable and confirmed Ebola cases were followed during the incubation period of 21 days.[100]
On 17 August, the Ministry of Health of the Democratic Republic of the Congo reported an outbreak of the Ebola-Bundibugyo variant[101] in the eastern region.[102] By 21 August, the WHO reported a total of 15 cases and 10 fatalities.[103] No evidence suggested that this outbreak was connected to the Ugandan outbreak.[104] By 13 September 2012, the WHO revealed that the virus had claimed 32 lives and that the probable cause of the outbreak was tainted bush meat hunted by local villagers around the towns of Isiro and Viadana.[105]
2014 outbreak
Main article: 2014 West Africa Ebola outbreak
In March 2014, an outbreak of the Ebola virus occurred in the Western African nation of Guinea.[106] This is the first Ebola virus outbreak registered in the region.[106] As of 10 April, 157 suspected and confirmed cases and 101 deaths had been reported in Guinea, 22 suspected cases in Liberia including 14 deaths, 8 suspected cases in Sierra Leone including 6 deaths, and 1 suspected case in Mali.[107][108] By late June 2014, the death toll had reached 390 with over 600 cases reported.[109] By 23 July 2014, the World Health Organization had reported 1201 confirmed cases including 672 deaths since the epidemic began in March.[110] On 31 July 2014, WHO reports the death toll has reached 826 from 1440 cases.[111]Emory University Hospital was the first US hospital to care for people exposed to Ebola.[112] Two American medical providers, Kent Brantly and Nancy Writebol, were exposed while treating infected patients in Liberia. Arrangements were made for them to be transported to Emory via speciality aircraft. Emory Hospital has a specially built isolation unit set up in collaboration with the CDC to treat people exposed to certain serious infectious diseases.[113][114][115] On 2 August 2014, Brantly was flown in to Dobbins Air Force Base in Marietta, Georgia, and transferred to Emory Hospital.[116]
History
For more about the outbreak in Virginia, US, see Reston virus.
Ebola virus was first isolated in 1976 during outbreaks of Ebola hemorrhagic fever in Zaire[117] and Sudan.[118] The strain of Ebola that broke out in Zaire has one of the highest case fatality rates of any human virus, roughly 90%.[119]The name of the disease originates from one of those first recorded outbreaks in 1976 in Yambuku, Democratic Republic of the Congo (then Zaire), which lies on the Ebola River.[117]
While investigating an outbreak of Simian hemorrhagic fever virus (SHFV) in November 1989, an electron microscopist from USAMRIID discovered filoviruses similar in appearance to Ebola in tissue samples taken from crab-eating macaque imported from the Philippines to Hazleton Laboratories Reston, Virginia.[120] Blood samples were taken from 178 animal handlers during the incident.[121] Of those, six animal handlers eventually seroconverted. When the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.[122]
In 1990, Hazelton Research Products' Reston Quarantine Unit in Reston, Virginia, suffered a mysterious outbreak of fatal illness among a shipment of crab-eating macaque monkeys imported from the Philippines. The company's veterinary pathologist sent tissue samples from dead animals to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Maryland, where a laboratory test known as an ELISA assay showed antibodies to Ebola virus.
Shortly afterward, a US Army team headquartered at USAMRIID went into action to euthanize the monkeys which had not yet died, bringing those monkeys and those which had already died of the disease to Ft. Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation, researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (REBOV) after the location of the incident.[123]
Some scientists also believe that the Plague of Athens, which wiped out about a third of its inhabitants during the Peloponnesian War, may have been caused by Ebola. However, these studies are conflicting, and point to other possible diseases such as typhoid.[124]
Society and culture
Given the lethal nature of Ebola, and since no approved vaccine or treatment is available, it is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use in biological warfare.[125][126]Other animals
In general, outbreaks of EVD among human populations result from handling infected wild animal carcasses. In general, declines in animal populations precede outbreaks among human populations. Since 2003, such declines have been monitored through surveillance of animal populations with the aim of predicting and preventing EVD outbreaks in humans.[127] Recovered carcasses from gorillas contain multiple Ebola virus strains, which suggest multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoir and animal populations.[128]Ebola has a high mortality among primates.[129] Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.[130] Outbreaks of EVD may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in 420 square kilometer Lossi Sanctuary between 2002 and 2003.[128] Transmission among chimpanzees through meat consumption constitutes a significant risk factor, while contact between individuals, such as touching dead bodies and grooming, is not.[131]
Domestic animals
Ebola virus can be transmitted to dogs and pigs.[132] While dogs may be asymptomatic, pigs tend to develop symptomatic disease.Research
Medications
Favipiravir looks like it may be useful in a mouse model of the disease.[13] Estrogen receptor drugs used to treat infertility and breast cancer (clomiphene and toremifene) inhibit the progress of Ebola virus in infected mice.[133] Ninety percent of the mice treated with clomiphene and fifty percent of those treated with toremifene survived the tests.[133] Given their oral availability and history of human use, these drugs would be candidates for treating Ebola virus infection in remote geographical locations, either on their own or together with other antiviral drugs.Antibodies
Main article: 2014 West Africa Ebola outbreak § Treatment
On 4 August 2014 an experimental drug, ZMapp, was first tested on humans. It was administered to two Americans who had been infected with Ebola. Both people appeared to have had positive results.[137][138]
Other treatments
Other promising treatments rely on antisense technology. Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the Zaire Ebola virus (ZEBOV) RNA polymerase L protein could prevent disease in nonhuman primates.[139][140]'
SOURCE: Wikipedia Free Encyclopedia









.jpg)
Comments